By Caitlin Carew
When we think of essential services during a disaster, things like clean water, food, medicines and emergency shelter come to mind.
But for a group of people who can often be relegated to the margins of society, continued access to needle exchange services is essential for their health and wellbeing.
Anne Rijnink of Massey University, supported by supervisor Associate Professor Denise Blake of Te Herenga Waka Victoria University of Wellington, recently studied the experience of people who inject drugs (PWID) on the South Island’s West Coast. With the support of people from the PWID community, they wanted to explore how disasters, including the COVID-19 pandemic, had impacted access to safe drug-using equipment in rural areas. They also wanted to gain an understanding of users’ likely vulnerability to natural hazard risks.
“Barriers to healthcare for people who inject drugs have been well documented, but as far as we are aware, this was the first study to look at access issues during disasters for people living in rural Aotearoa,” says Denise.
The Needle Exchange Programme (NEP) is a compassionate healthcare service driven by peers who take a pragmatic approach to reducing drug-injecting harm. NEPs recognise that abstinence from drugs can be an unrealistic goal for some people, and it’s therefore important to provide them with sterile injecting equipment to reduce their risk of contracting blood-borne virus such as HIV/AIDs, and the Hepatitis B and Hepatitis C virus.
On the West Coast, NEP services are provided to PWID by mobile outreach service, by staff based in Nelson and through pharmacies.
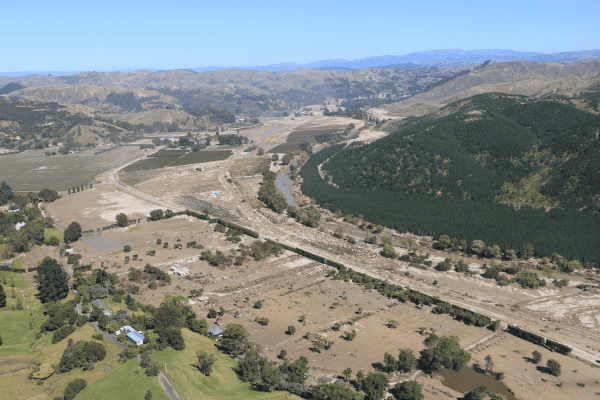
The success of the NEP outreach service on the West Coast is threatened by natural hazard risks. For instance, the region would be significantly impacted by a large earthquake on the Alpine Fault, with likely disruption to roading links. Over the last few years we’ve seen how vulnerable the West Coast is to flooding, particularly Westport which experienced major, disruptive flooding in July 2021 and February 2022.
Covid-19 also posed challenges for the NEP mobile outreach service. “Although the service was classified as an ‘essential service’ during the Level 4 lockdown, there were still disruptions to accessing safe equipment.”
Previous research has illustrated how disasters can exacerbate existing inequalities. It is likely that people in the drug-injecting community on the West Coast would be disproportionately impacted by a natural hazard event, due to being a marginalised group and, for some, experiencing socio-economic disadvantage.
“We also know they are less likely to have the ability to prepare for a disaster and more likely to live in substandard or insecure housing.”
The research was inspired by questions from the community themselves, who had concerns about accessing NEP services following a flood. They wanted to ensure there were emergency plans in place. To understand vulnerabilities of the service, and what could be done about those access vulnerabilities, researchers conducted interviews with fourteen participants: 13 PWID from across the West Coast region, and one Nelson-based NEP staff member.
Four main themes were identified.
Firstly, the researchers identified factors that could hinder outreach accessibility in a disaster, including infrastructure and equipment costs.
They identified the importance of peers, which includes social capital, practical support and key contact networks.
The gained an understanding of the social stigma faced by participants, including fear of stigma from healthcare professionals and emergency managers in a disaster situation.
Finally, they gathered the most frequently mentioned solutions to NEP service disruptions during disasters.
Researchers concluded that continued access to NEP services is essential during disasters.
A range of potential solutions to accessibility concerns arose, such as liaising with emergency management personnel, finding safe community spaces to store drug-injecting equipment and ensuring access to cost-free equipment. Another possibility, as exists in static NEP exchanges, are electronic dispensers. They also suggest that PWID be empowered to collaborate with health authorities and emergency management personnel to establish backup plans.
Overall, the researchers advocate for a needs-based, stigma-free approach to harm-reduction, and that emergency management practices need to better cater for groups with specific requirements.
“Importantly, this requires a paradigm shift away from the ‘one-size-fits-all’ approach to emergency management largely practised in Aotearoa New Zealand,” says Denise.
The team also recommend ongoing research to continue to explore the views and experiences of PWID to determine how best to support them, on their terms, during disasters.
The research was published as Rijnink, A., Blake, D., Groot, S. et al. Accessing needle exchange services in disasters for remote areas of Aotearoa New Zealand. Harm Reduction Journal 19, 145 (2022). You can access the article here.